
Enhancing Revenue Growth through Real-Time Insurance Eligibility Verification
WellTrust recognizes the difficulties healthcare providers encounter when dealing with time-consuming insurance eligibility verification procedures, which often result in claim denials.
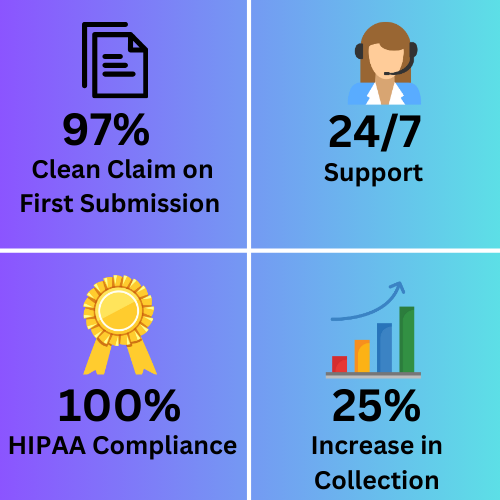
By prioritizing precision, effectiveness, and minimizing denials, WellTrust offers a comprehensive range of real-time insurance eligibility verification services that seamlessly integrate with your current systems. This integration streamlines workflows, enabling you to concentrate on delivering exceptional patient care.
Our team of experts is dedicated to relieving you from the complexities of documentation, empowering you to grow your practice while reducing claim denials by an impressive 30%.
Benefits of Verifying Insurance Coverage:
- Enhancing point of service collections (Co-pays, Out Of Pocket, etc.)
- Can lead to a more efficient revenue cycle,
- Reducing the risk of claim denials due to lack of coverage, and ultimately reducing risk factors while
- Improving the patient experience. Additionally,
- Simplifying workflow can lead to reduced
- Rework of claims and decreased account receivables days, while also providing alerts about self-pay patients.
How WellTrust will do it?
- The executives at WellTrust will retrieve the patient’s insurance details either from the appointment schedule for the following day or the practice can opt to send it via email in a secure file format.
- We utilize various methods to verify benefits and eligibility based on the insurance payer, including accessing websites, utilizing an Automated Voice Response System, and contacting the Customer support center.
- Our verification process includes checking the specific benefits or details listed below, as and when requested by the provider.
- Detailed information will be logged as notes in the individual patient’s account.
- If the coverage is discontinued or the service is not included, the patient will be contacted and notified accordingly. They will also be asked if they have any other insurance coverage options available.
- The practice manager receives a comprehensive daily report containing verified notes on all the patients
