Optimize Medical Claims Processing through Denial Management Services.
The financial stability and operational efficiency of healthcare providers can be severely impacted by unforeseen denials, resulting in delayed or reduced reimbursements. Explore how our expertise can assist you in navigating the challenging landscape of denial management, allowing you to join the 72% of healthcare organizations that witness improved operational efficiency through the outsourcing of denial management.
At WellTrust, we comprehend the vital significance of proactively dealing with denials to maximize your revenue stream. With our extensive 12 years of experience, we have developed a data-driven approach that empowers healthcare providers to recover up to two-thirds of rejected claims, leading to significant improvements in their financial outcomes.
Expertly Guiding You Through Every Stage: Streamlined Denial Management in the Healthcare Sector.

01
Needs Assessment Perform a meticulous assessment of your denial management system, identify the challenges faced, and tailor our services to suit your individual requirements, thereby maximizing the effectiveness of our partnership.

02
Denial Prevention Strategies Maximize your revenue potential by taking proactive steps to prevent denials. Ensure that your claims are clean, coding is accurate, documentation is thorough, and payer requirements are met.
03
Claims Scrubbing Thoroughly inspects each claim, meticulously rectifying any errors or omissions in the information provided, with the goal of minimizing denials and streamlining the processing of claims.

04
Denial Analysis Conduct an extensive assessment of denials, classify them methodically, uncover emerging trends, and trace the root causes to effectively tackle underlying problems and proactively prevent future denials.
05
Appeals Management Promptly initiate appeals on your behalf, collect relevant documentation, work closely with providers, and submit carefully prepared appeals to achieve favorable outcomes in claim resolution.

06
Technology and Reporting Maximize the potential of advanced technology and analytics to effectively track denials, closely monitor trends, and generate insightful reports that enable informed decision-making and foster improved financial results.

07
Ongoing Support and Collaboration Maintain transparent communication and work closely with your team, conducting periodic performance evaluations to refine strategies for ongoing enhancement and long-term prosperity.

08
Tracking and Appealing Denials Generate appeal letters efficiently by utilizing statutes as a basis. Ensure prompt prioritization, tracking, and appealing of denials. Stay updated on the status of claim appeals through cutting-edge tracking methods.
Why WellTrust for Denial Management Services?
★ Increased Revenue
Our proactive approach to managing denials and strategically appealing them results in increased revenue realization for your healthcare organization.
★ Streamlined Operations
By entrusting WellTrust with your Denial management in healthcare, your internal teams can dedicate their attention to patient care and core competencies, thereby improving overall operational efficiency.
★ Reduced Administrative Burden
Our services alleviate the burden of administrative tasks, enabling your staff to allocate more time towards critical responsibilities.
★ Credit Balance Services
Efficiently handle credit balances utilizing our specialized knowledge, ensuring adherence to regulations and fostering patient confidence through prompt and precise reimbursements.
★ Improved Cash Flow
Enhancing cash flow and ensuring financial stability for your organization can be achieved by reducing denials and expediting revenue cycles.
★ Enhanced Compliance
Our extensive knowledge of industry regulations when managing your denial management in the healthcare sector guarantees that your claims adhere to payer requirements, thereby minimizing the likelihood of compliance violations.
★ Expert Support
By collaborating with Med Denial Solutions, you gain access to a group of denial management specialists and industry professionals who are committed to enhancing your revenue and financial results.

Achieve Your Revenue Goals with Denial Management Services from WellTrust
Healthcare organizations are currently grappling with the complexities of the healthcare industry, particularly when it comes to unresolved claims denials. These denials have become a significant burden, with hospitals losing an average of $5 million each year. To alleviate this financial strain, it is imperative for healthcare organizations to outsource denial management to a trusted partner.
By partnering with us, you can optimize your denial management services and reap the benefits of our innovative problem-solving approach. Our denial management services have proven to be highly effective, resulting in a remarkable 30% reduction in denied claims. Furthermore, by utilizing our services, you can expect an average annual increase in revenue of 20%.
Don’t let unresolved claims denials continue to drain your resources. Join forces with us and experience the positive impact of our denial management services on your healthcare organization’s financial stability
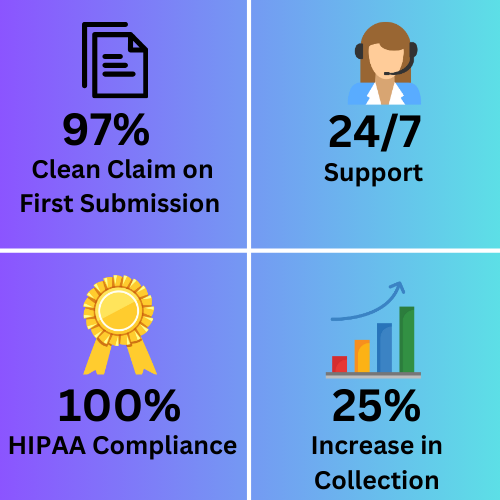
The Medical Billing Advantages
Operational Bandwidth – Boost by
30%
Claim Denials – Reduce by
95%
WellTrust: Transforming Healthcare with Successful Case Studies
Explore the tangible effects of WellTrust’s denial management services by delving into our captivating case studies. We are dedicated to presenting the triumphs of our contented customers who have accomplished extraordinary outcomes in enhancing revenue and simplifying operations.